Pregnancy can be a difficult time for any woman, but it can be especially hard for those who are dealing with an addiction or substance use disorder (SUD) or specifically an opioid use disorder (OUD). With opioid use on the rise in the United States, more pregnant women are turning to medication for addiction treatment (MAT) to help them manage their addiction during pregnancy. One of the most common medications used to treat OUD during pregnancy is Suboxone, but is it safe? In this article, we will cover Suboxone and its effects on both mother and baby during pregnancy.
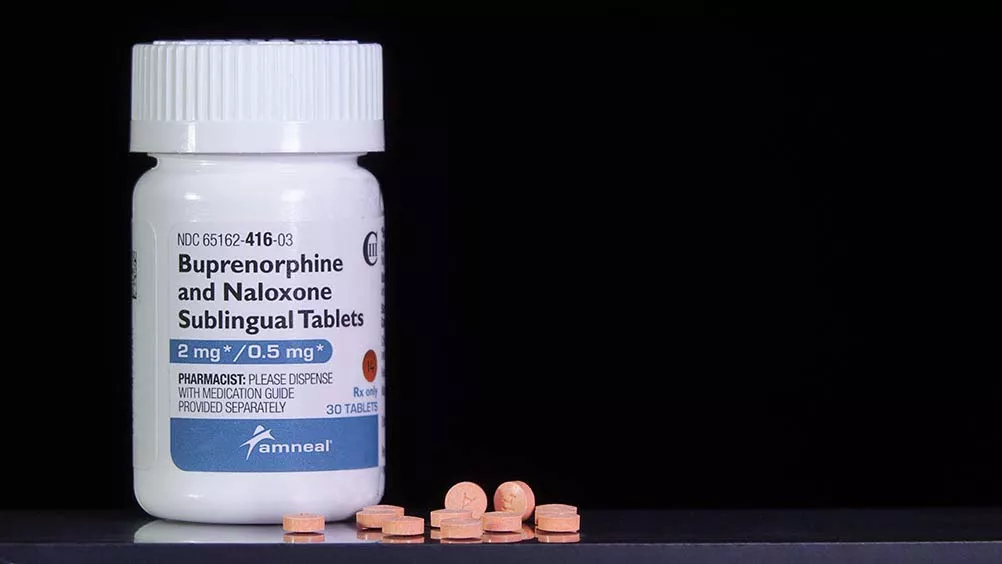
Suboxone is a prescription medication used in the treatment of opioid use disorder. It contains buprenorphine and naloxone in a ratio of 4:1. Buprenorphine is a partial opioid medication that blocks the opioid receptors and reduces cravings. The second ingredient, naloxone, aids in the reversal of opioid effects and prevents the risk of misuse. Together, these medications work to minimize withdrawal symptoms associated with opioid addiction. Suboxone is available in sublingual tablets or film strips placed under the tongue, gums, or cheek to dissolve. Suboxone takes effect 30 to 60 minutes after administration, and the effects can last between 48 to 72 hours (depending on the dose).
According to the National Institute on Drug Abuse (NIDA), Suboxone is a safe medication during pregnancy. Historically, Subutex, a pure buprenorphine medication, was the preferred medication during pregnancy since early studies were only conducted using buprenorphine instead of the buprenorphine/naloxone combination. But recent studies indicate that Suboxone is also safe for mothers as it is for their babies. Suboxone combined with behavioral therapy effectively lowers relapse rates and opioid overdoses while improving birth outcomes in opioid-dependent mothers.
Babies born to mothers who used Suboxone correctly during pregnancy experienced minor fetal distress and other symptoms after birth. While Suboxone is generally safe, babies born to mothers who have used Suboxone can develop neonatal abstinence syndrome (NAS), a set of withdrawal symptoms experienced by newborn babies after being exposed to opioids in the womb. Neonatal abstinence syndrome is an expected, common, and treatable condition, and in most cases, any opioid withdrawal that the baby experiences is relatively mild.
Neonatal abstinence syndrome (NAS) is a set of withdrawal symptoms experienced by newborn babies after being exposed to opioids in the womb. While Suboxone is safely prescribed during pregnancy, babies born to mothers who have used Suboxone can develop neonatal abstinence syndrome (NAS). This condition occurs when any form of opioids are used during pregnancy, including opioid medications used during opioid addiction treatment. Neonatal abstinence syndrome is an expected, common, and treatable condition.
According to the National Center for Biotechnology Information (NCBI), neonatal abstinence syndrome include withdrawal symptoms such as:
It’s important to note that NAS caused by Suboxone is short-lived and less intense than NAS caused by the overuse of prescription opioids or heroin. And as such, the benefits of Suboxone generally far outweigh the risks involved. The baby may be safer exposed to Suboxone (which is helping the mother manage her addiction during pregnancy) than being exposed to an opioid such as heroin.
Methadone is an alternative medication to Suboxone during pregnancy. At present, Suboxone is classified as a category B medication that’s used routinely and safely during pregnancy. And methadone is a category C medication, which is relatively safe during pregnancy. Methadone is classified as a category C medication because of the risk of respiratory depression in newborns and the possibility of NAS. And category C medications are only prescribed if the potential benefit outweighs the risk to the fetus. According to a recent study conducted by the National Institutes of Health (NIH), the buprenorphine in Suboxone was superior to methadone in reducing withdrawal symptoms in newborn babies.
Unlike Suboxone, which is prescribed through any healthcare practitioner licensed to prescribe Suboxone, methadone prescriptions require regular visits to a methadone clinic, which can be inconvenient, especially as you go further into your pregnancy.
The right treatment option and medication are ultimately dependent on the severity of your opioid dependence and other health conditions. It’s important to seek medical advice about what’s best for your situation.
It’s not recommended to discontinue Suboxone use during pregnancy unless you are advised and supervised by your doctor. Because Suboxone is a partial opioid medication, stopping use could result in acute opioid withdrawal, which can present dangers to an unborn baby, such as fetal distress, preterm labor, and miscarriage. Additionally, newborns will have strong cravings for opioids if a proper plan for tapering is not in place. In most cases, it’s advisable to keep taking the medication during pregnancy unless your doctor suggests otherwise.
During pregnancy, your doctor may suggest you either reduce or keep your Suboxone dose. Your Suboxone dose will be determined based on your present health condition and where you are in your rehabilitation. As a result, working with your health care practitioner to decide your daily Suboxone dosage is critical.
Research indicates that buprenorphine in Suboxone passes into breast milk. But since the amount that passes is minimal, infants will not experience withdrawal symptoms after they are weaned off breast milk. Studies reveal that Suboxone is well tolerated in nursing mothers, and hence discontinuation may not be necessary.
Breastfeeding during Suboxone treatment is safe as long as:
Pregnant women with opioid use disorder should consult with their doctor to determine if Suboxone is the right medication for them. Suboxone should be used as part of a comprehensive treatment plan that includes obstetrical care and behavioral therapy. The goal of Suboxone treatment during pregnancy is to reduce the risk of relapse and overdose while improving maternal and fetal outcomes. If you’re already on Suboxone, your doctor will be able to determine whether you should continue taking Suboxone or switch to Subutex.
If you are seeking help with your loved one’s addiction, contact us today or complete our quick contact form below, to speak with an addiction treatment specialist.
If you need help with your substance use disorder, we are here to help you build your confidence and momentum towards the future you want. We provide treatment services for adults with alcohol, opioid, and other substance use disorders. We are currently located in Louisiana, Massachusetts, North Carolina, New Jersey, Ohio, Texas, and Washington.
 How Long Does Suboxone Stay in Your System?
How Long Does Suboxone Stay in Your System?
 Naltrexone vs. Suboxone – How are They Different?
Naltrexone vs. Suboxone – How are They Different?
 Virtual Addiction Treatment: is it as Effective as In-Person Treatment?
Virtual Addiction Treatment: is it as Effective as In-Person Treatment?