Understanding the stages of alcohol withdrawal and who’s at risk of dangerous symptoms will help you prepare for the journey. While some people find success detoxing on their own, having professional help to manage symptoms will increase the chances of a safe and successful recovery.
Alcohol withdrawal syndrome (AWS) is a set of symptoms that occur when someone who has been drinking heavily for an extended period suddenly stops or significantly reduces their alcohol consumption. When the body becomes dependent on alcohol, it goes into a state of imbalance once the substance is removed.
Alcohol withdrawal is not the same for everyone. The severity and presence of withdrawal depend on several factors, including the duration and amount of alcohol consumption, individual health conditions, and previous history of withdrawal. While most cases are mild, if you experience severe or acute withdrawal, seek immediate medical attention, as symptoms can be life-threatening if left alone.
Alcohol withdrawal typically follows a predictable timeline, with symptoms emerging within hours after you stop drinking and lasting 7 to 10 days. There are three potential stages of alcohol withdrawal, although most people will only experience the first stage. Medical assistance is always recommended but will become necessary if symptoms progress beyond the first stage.
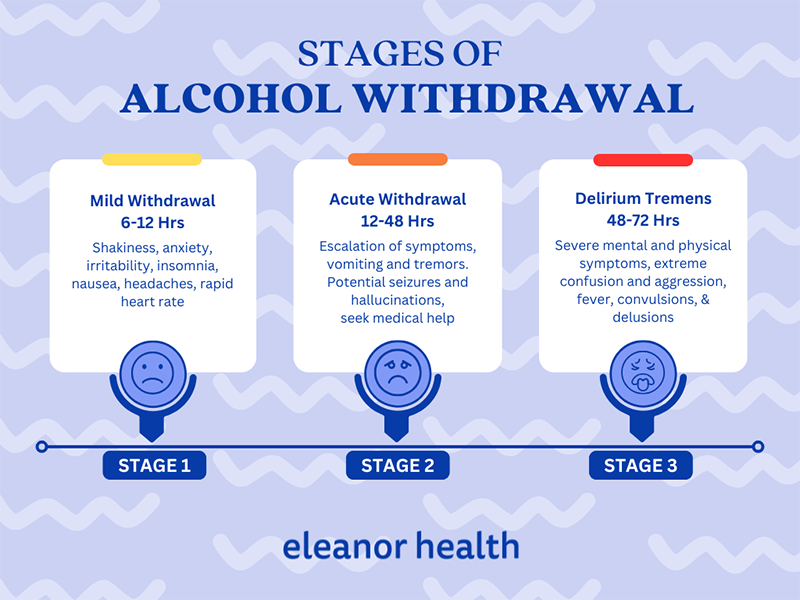
The first stage of alcohol withdrawal often begins within 6 to 12 hours after the last alcoholic beverage is consumed. During this phase, individuals may experience mild to moderate symptoms, including:
While these symptoms can be uncomfortable, they are generally not life-threatening. Most people will recover after these symptoms clear up, which can take up to 7 days.
In some cases, symptoms will escalate between 12 and 48 hours after the last drink, generating a severe form of withdrawal characterized by seizures and hallucinations. About 5% of people going through alcohol withdrawal without medical treatment will enter the second stage. Hallucinations and seizures during acute withdrawal represent emergencies and medical attention should be sought immediately.
Delirium tremens (DTs) is the most severe and third stage of alcohol withdrawal. It typically occurs between 48 and 72 hours after the last drink, and lasts 2 to 3 days. DTs are characterized by a rapid onset of severe mental and physical symptoms, including:
DTs can be life-threatening if left untreated and require immediate medical intervention. Only a small percentage (approximately 5%) of individuals undergoing alcohol withdrawal will experience DTs.
There are certain factors that may increase the risk of acute withdrawal symptoms like seizures and DTs. If any of these factors apply to you, consult with a doctor or go to the emergency room before you stop drinking. You may need inpatient care to detox safely and manage symptoms.
Medical detoxification or detox for alcohol is a process designed to help individuals safely withdraw from alcohol under medical supervision. It can be done either inpatient or outpatient, depending on your health, needs, and personal preferences.
If you’ve experienced physical danger during detox in the past, it’s a strong indicator that you need medical assistance at a clinic or other inpatient setting. Healthcare professionals will monitor your vital signs and manage any complications that arise.
Mild alcohol withdrawal can often be managed at home with a supervised medical detox. In this case, a medical team will prescribe you medications and set up a regular monitoring schedule to check on your progress and provide guidance. Outpatient detox programs like Eleanor Health can help you manage symptoms and monitor your progress without disrupting your daily routine.
Benzodiazepines are the first-line treatment for alcohol withdrawal due to their effectiveness and safety profile. They help alleviate withdrawal symptoms by calming the central nervous system and preventing seizures. Commonly used benzodiazepines include:
Anticonvulsants can be used as alternatives to benzodiazepines in managing alcohol withdrawal symptoms. They can also be used together with benzodiazepines to enhance the effectiveness of the treatment. Anticonvulsants used to treat alcohol withdrawal include:
Once detoxification is complete, other medications may be prescribed to help maintain abstinence and prevent relapse. These include:
Withdrawal is a medical issue, not a personal failure. Medical detoxification makes the process safer, more manageable, and greatly increases the chances of long-term success, but it’s just the first step in your journey.
Recovery from alcohol use disorder is a journey that is best undertaken with the support of a caring and understanding community. Seeking out and embracing the support of loved ones, peers in recovery, and professional addiction treatment providers can significantly enhance the chances of long-term success. You don’t have to face addiction alone. Join Eleanor Health as one of our members and join the community.
 Benefits of Switching From Methadone To Suboxone
Benefits of Switching From Methadone To Suboxone
 Virtual Addiction Treatment: is it as Effective as In-Person Treatment?
Virtual Addiction Treatment: is it as Effective as In-Person Treatment?
 Does Insurance Cover Online Rehab and Medication-Assisted Treatment?
Does Insurance Cover Online Rehab and Medication-Assisted Treatment?