Opioid use disorder (OUD) and alcohol use disorder (AUD) remains a public health crisis in the United States and globally. Three million Americans and 16 million individuals worldwide suffer from opioid use disorder. And an estimated 14.5 million Americans ages 12 and older suffer from alcohol use disorder. These illnesses are chronic diseases that affect people from all walks of life.
In light of the growing concern, governments and medical institutions worldwide are investing significant resources into developing and promoting innovative approaches to address substance use disorders (SUDs). And medications for addiction treatment (MAT) is one of the strategies that has emerged as a result of such attempts.
The Substance Abuse and Mental Health Services Administration (SAMHSA) describes the medication for addiction treatment as a “whole-person” approach to addiction treatment that includes FDA-approved medications, counseling, and behavioral therapies. Medication for opioid use disorder (MOUD) and alcohol use disorder is clinically proven to help individuals overcome addiction and maintain long-term sobriety.
Some of the most commonly used FDA-approved medications for opioid use disorders are Naltrexone and Suboxone. And studies reveal both to be effective in treating opioid addiction. However, they tend to differ from each other regarding their nature, how they work, and their potential risk for overdose and withdrawal.

Naltrexone is a prescription medication that has been in use for many years for treating alcoholism and opioid addiction, two of the most common forms of substance use disorders in the U.S. There are three mechanisms via which naltrexone works. It helps counteract the effects of opiates, reduce cravings for alcohol or opiates, and prevent relapse by decreasing with the temptation to keep drinking.
Naltrexone can help people with substance use disorders by lowering the risk of relapse and enhancing focus on other aspects of rehabilitation. Naltrexone is an opioid antagonist (inhibitor) that is relatively pure, long-lasting, and non-addictive.
Naltrexone is available in pill form (ReVia and Depade) for alcohol use disorders and an injectable form (Vivitrol) for alcohol addiction and opioid addiction. The pill form is usually prescribed to be taken daily at home or in a clinical setting, while the injectable form is administered once a month by a healthcare provider. Naltrexone can be prescribed and administered by any healthcare practitioner licensed for dispensing medications.
Since it tends to create serious withdrawal symptoms in people who have opioids in their system, naltrexone can only be recommended to individuals who haven’t taken opioids for 7-14 days before therapy. This also includes those who have used methadone in the past and are switching to naltrexone. Individuals currently using alcohol, on the other hand, can be prescribed naltrexone.
Even though naltrexone is regarded as a useful component in treating alcohol and opioid addiction, it may not be the best treatment option for everyone. As a result, it’s critical to obtain medical guidance before starting naltrexone medication.
Naltrexone is recommended for people who are:

Buprenorphine and naloxone are the two main ingredients of Suboxone. Suboxone contains buprenorphine, a partial opioid agonist that blocks opiate receptors and reduces cravings. Naloxone, the second component, serves to counteract the effects of opioids. Both components work together to alleviate the withdrawal symptoms that accompany opioid addiction.
This medication is available as an oral film that’s placed under your tongue (sublingual) or between your gums and cheeks (buccal). Within minutes, the film melts in your mouth and enters your bloodstream. Oral tablets are also available for this medication.
Suboxone works by tightly attaching to the same brain receptors as other opioids. This function helps people move from a life of addiction to a life of sobriety by dulling intoxication and preventing cravings. Suboxone is a schedule III controlled substance that can only be prescribed for MOUD purposes by doctors who have received special training and certification from the U.S. federal government.
Suboxone for opioid addiction, like naltrexone, may not be the best treatment option for everyone. Tell your doctor if you’ve ever had any of the following conditions to ensure Suboxone is safe for you:
If you are pregnant or breastfeeding, consult your doctor before using Suboxone. If you notice your nursing baby appears drowsy or breathing slowly, call your doctor immediately.
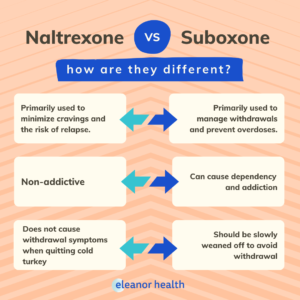
Naltrexone functions by binding to opioid receptors and inhibiting their effects. While in recovery, this minimizes cravings and the risk of relapse. During the recovery process, naltrexone is primarily used to avoid relapses. And as a result, it’s only recommended or prescribed when a person has not used opioids for at least 7-14 days completed opioid detox and is no longer physically dependent on opioids.
On the contrary, Suboxone for opioid addiction treatment is primarily used to manage withdrawal, prevent relapses and overdoses. It’s prescribed for use at the beginning of the withdrawal phase and is continued for a considerable period afterward to prevent relapses.
The buprenorphine in the medication attaches itself to the opioid receptors and blocks other opiates from occupying them. Since buprenorphine is a partial opioid agonist, this function reduces cravings and the intensity of withdrawal symptoms and makes long-term sobriety possible. And the main purpose of naloxone is to block the activation of opiate receptors and prevent the misuse of Suboxone.
Naltrexone is a non-addictive medication that does not bind to opioid receptors. As a result, stopping cold turkey will not result in any withdrawal symptoms. When used while under the influence of opioids, however, it might cause sudden opiate withdrawals. This is caused by the fact that naltrexone binds to opiate receptors in the brain and blocks their effects almost immediately, causing withdrawal symptoms to emerge rapidly rather than gradually. Sudden opiate withdrawal can be more intense and include symptoms such as:
As such, individuals are advised to wait for at least seven days since the last use of short-acting opioids and 10-14 days for long-acting opioids before receiving naltrexone treatment. They should also inform their healthcare providers about the use of any opioid medications currently in use.
Unlike naltrexone, Suboxone is an opioid that can cause physical and psychological dependence when used for a long period. And quitting cold turkey can trigger withdrawal symptoms that can be quite similar to other opioids. The symptoms of Suboxone withdrawal can vary in intensity and duration depending on factors such as the dosage of the medication and period of use.
Some of the withdrawal symptoms of Suboxone are:
Healthcare practitioners should be able to prevent such withdrawal symptoms by slowly tapering the medication’s doses. Hence, individuals who wish to stop using suboxone are advised to seek support and guidance from their physician before quitting.
Although it’s technically possible to overdose on naltrexone, this is highly uncommon. Since naltrexone does not cause euphoria in the same manner that most other opioids do, people are less likely to increase the effects by taking excessive doses. However, it’s possible to experience an overdose if individuals consume large doses of opioids to overcome the blocking action of naltrexone.
Some of the symptoms of an opioid overdose are:
Suboxone, on the other hand, can induce an overdose when taken in high quantities or used beyond the doctor’s prescription. This is because Suboxone is an opioid, and attempting to increase its effects by taking large amounts of the medication can overload the body with toxic substances.
Some of the symptoms of a Suboxone overdose are:
Overdoses can result in serious injuries, coma, and even death. So it’s important to seek immediate medical attention if you experience any of the following symptoms.
Despite their differences, naltrexone and Suboxone are praised in the medical community for their effectiveness in treating opioid addiction. However, it’s vital to remember that such medications will not assist individuals in overcoming their opioid addiction on their own. These medications are highly effective in opioid maintenance treatment only when combined with other aspects of an addiction treatment program.
If you are seeking help with your loved one’s addiction, contact us today to speak with an addiction treatment specialist.
If you need help with your substance use disorder, we are here to help you build your confidence and momentum towards the future you want. We provide treatment services for adults with alcohol, opioid, and other substance use disorders. We are currently located in Louisiana, Massachusetts, New Jersey, North Carolina, Ohio, Texas, and Washington.
 Naltrexone Implant – How Can it Help You?
Naltrexone Implant – How Can it Help You?
 How Long Does Naltrexone Take to Work?
How Long Does Naltrexone Take to Work?
 Benefits of Online Addiction Treatment
Benefits of Online Addiction Treatment