Lexapro is a brand name for the medication Escitalopram, a selective serotonin reuptake inhibitor (SSRI) used to treat depression and anxiety disorders. This antidepressant medication was first approved by the US Food and Drug Administration (FDA) in August 2002 and sold in the United States soon after approval.
Lexapro primarily treats major depressive disorder (MDD) and generalized anxiety disorder (GAD) in adults. It’s also used off-label to treat other conditions such as post-traumatic stress disorder (PTSD), social anxiety disorder, obsessive-compulsive disorder (OCD), and panic disorder. You should only use Lexapro under the supervision of a healthcare provider, and it may take several weeks before feeling the full effects of the medication.
Lexapro is an SSRI that increases the neurotransmitter serotonin levels in the brain. Serotonin is a chemical messenger that regulates mood, anxiety, and other functions in the brain.
Individuals with anxiety or depression disorders often have low serotonin levels. SSRIs like Lexapro work by inhibiting serotonin reuptake, meaning more serotonin is available to bind to receptors in the brain. This increase in serotonin can help improve mood and reduce anxiety symptoms.
The use of Lexapro should be as directed by a healthcare provider, and the drug is available in three different forms;
It’s vital to take Lexapro at the same time each day to maintain an even level of the medication in your bloodstream. Taking Lexapro with a meal or glass of water is also recommended to minimize stomach upset.
The onset of side effects from Lexapro (Escitalopram) can vary from person to person. Some people may experience side effects shortly after starting the medication, while others may not experience side effects until several weeks into treatment.
These side effects are usually temporary and may improve over time or with a change in the time of day when the medication is taken.
Serious side effects, such as changes in mood or behavior, suicidal thoughts, agitation, or restlessness, may occur at any time during treatment, but they are rare. If you experience any side effects that are persistent or severe, contact your healthcare provider immediately.
Healthcare providers don’t recommend drinking alcohol while taking Lexapro. Alcohol can interact with Lexapro and may increase the risk of side effects such as dizziness, drowsiness, and impaired judgment.
Drinking alcohol can interfere with Lexapro’s effectiveness. It may worsen symptoms of anxiety and depression and may lead to addiction or other mental health issues. Consuming alcohol while taking Lexapro may increase the risk of developing a serious condition called serotonin syndrome, a rare but potentially life-threatening condition.
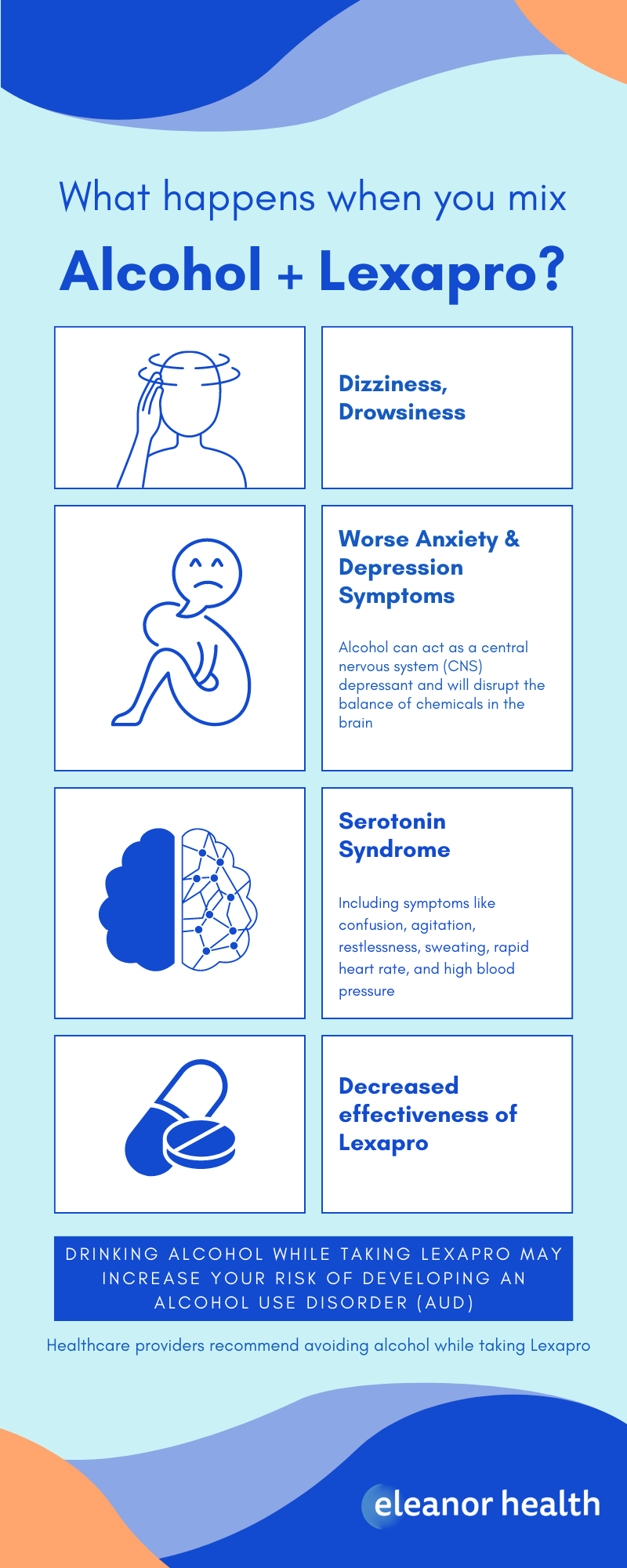
Mixing alcohol and Lexapro (escitalopram) can lead to several potential side effects, including:
The effects of alcohol on depression and anxiety can vary depending on the amount consumed and the individual. In the short-term, alcohol can act as a central nervous system (CNS) depressant, which can lead to a decrease in anxiety and a temporary feeling of euphoria. However, the effects are short-lived; in the long term, alcohol can worsen symptoms of depression and anxiety.
Regular or heavy alcohol consumption can disrupt the balance of chemicals in the brain, making depression and anxiety symptoms worse. Additionally, heavy alcohol use can lead to several physical and mental health problems that can further exacerbate symptoms of depression and anxiety.
Drinking alcohol as a way to cope with depression and anxiety is not healthy, and it can worsen the condition. If you have depression or anxiety and you’re drinking alcohol, talk to your healthcare provider about it. They can help you develop a plan to manage your condition safely and healthily.
There is a risk of developing alcohol use disorder (AUD) while taking Lexapro (escitalopram), especially if you have a history of substance use or addiction. Alcohol use disorder is characterized by a pattern of alcohol consumption that leads to significant impairment or distress.
Taking Lexapro does not increase the risk of developing a drinking problem directly. However, people who are taking Lexapro may be more likely to drink alcohol as a way to cope with their symptoms of depression or anxiety, which can lead to addiction over time.
If you notice any signs of addiction, such as difficulty controlling alcohol consumption, continued drinking despite adverse consequences, or withdrawal symptoms when you stop drinking, seek professional help.
Consult your healthcare provider about when it’s safe to start drinking alcohol after stopping Lexapro. The time frame can vary depending on the individual and the reason for stopping the medication.
Generally, it’s recommended to wait at least a couple of weeks after stopping Lexapro before drinking alcohol. Lexapro is an antidepressant medication that can take some time to completely clear from your system, and drinking alcohol while taking the medication can increase the risk of side effects and interactions.
If you were struggling with alcohol use disorder (AUD) or addiction before taking Lexapro, it’s best to avoid drinking altogether, or at least for a more extended period. Addiction is a chronic relapsing disorder, and stopping Lexapro does not remove the underlying addiction.
It’s important to remember that abruptly stopping Lexapro may cause withdrawal symptoms. Talk to your healthcare provider before stopping Lexapro or drinking alcohol. They can help you develop a plan to stop the medication safely and advise you on how to avoid or limit alcohol consumption.
If you think you have a problem with depression, anxiety, or alcoholism, seek help as soon as possible from Eleanor Health. We provide treatment services for adults with opioid, alcohol, and other substance use disorders, virtual therapy, and counseling.
Contact us today, as Eleanor Health is here to help you build your confidence and momentum toward the future you want. We are currently located in Louisiana, Massachusetts, North Carolina, New Jersey, Ohio, Texas, and Washington.
 The Link Between Anxiety and Alcohol
The Link Between Anxiety and Alcohol
 What are SSRIs?
What are SSRIs?
 What is Lexapro? (Escitalopram)
What is Lexapro? (Escitalopram)