Although there are various tools and practices one can use to decrease anxiety and depression, the symptoms of these mental illnesses are sometimes too strong to fight without the help of medication. This is why professionals recommend a combination of therapy and medication if your symptoms interfere with your life and responsibilities for two weeks or more.
Anxiety is a natural, normal, and healthy feeling. It derives from our innate human response to potential dangers. Anxiety developed as a survival instinct during early human history. Some call this our “caveman response” to potential threats. Nowadays, we are more likely to feel anxiety before an exam or job interview versus fighting off animals when hunting for food! However, when anxiety presents itself in response to stimuli that are not dangerous or threatening and becomes disruptive to your daily functioning, it can turn into an anxiety disorder.
Generalized Anxiety Disorder (GAD): The psychological and physiological experience for people with GAD has both significant and persistent consequences, including feelings of worry and dread; a strong tendency to ruminate or have inescapable, negative thoughts; and physical symptoms like agitated behavior, restlessness, and many more. GAD means that most things can generate anxiety – sometimes it might come on suddenly or “out of nowhere”. Anxiety has an important function to make humans pay attention and stay alert in a potentially dangerous situation, but when a person has GAD, that biochemical reaction is more sensitive, more severe, and longer lasting compared to someone without an anxiety disorder.
Social Anxiety Disorder: Social Anxiety Disorder symptoms are similar to GAD, except the anxiety response is rooted in social situations, particularly busy or chaotic spaces like shopping malls, festivals, bars, or even classrooms. Similar to GAD, someone with social anxiety disorder can experience thoughts, feelings, and a range of physical symptoms that manifest in significant ways.
Panic Disorder and Anxiety Attacks: Panic attacks are very sudden, extreme fear responses to something in a person’s environment, which can include an internal experience (like a memory), and someone that regularly experiences these attacks likely has a panic disorder. Panic attacks, as their name implies, are very overwhelming, involving mental and physical experiences like extreme dread and a distinct sense of feeling smothered (often leading to hyperventilating.
Depression is a serious mental illness that negatively impacts how one feels, thinks, and acts regarding their experiences. In July 2022, 23.2% of Americans ages 18 and older reported experiencing persistent symptoms of depressive disorder. That’s over ⅕ of the US population. From these statistics, it’s safe to say that depression is a disorder that affects a large portion of our population. Therefore it is essential to become aware of depression causes, symptoms, and treatment options.
Like many mental disorders, various types of depression have different causes. Here are the most common types of depression and how they can appear:
Situational Depression: This type of depression does not count as disordered depression or sadness. Situational depression refers to the melancholy mood all people get into after a distressing event. The depressed mood you feel in situational depression is in direct response to an event and typically subsides over time. For example, it is typical for someone to feel depressed after the death of a family member or a divorce. Through the passage of time and/or support, situational depression becomes manageable and eventually passes.
Major Depressive Disorder (MDD): People who suffer from major depressive disorder feel persistent depressive moods most of the time. Common symptoms are losing interest in what once was exciting, feeling sluggish and unmotivated, and having trouble making decisions. People with MDD also experience physical symptoms like weight loss/gain, lack of energy, and slowed body movements.
Seasonal Depression or Seasonal Affective Disorder (SAD): People with SAD feel the same symptoms of major depressive disorder, except only within particular seasons. For most people, symptoms of SAD flare up in the winter months. This is explainable by the wealth of research finding a solid association between shorter days/lack of sunlight and depression.
Persistent Depressive Disorder: Previously called “dysthymia,” this disorder is classified as experiencing depression symptoms for two consecutive years. Although people with this disorder may have periods of major depression, their typical symptoms are usually less severe, although long-lasting. Postpartum Depression: Postpartum depression is the depression a person may experience after childbirth. This is not to be confused with “baby blues,” which have similar symptoms to postpartum depression but only last for about a week after birth. Postpartum depression can start during pregnancy and last many months after giving birth. Symptoms like severe mood swings, feelings of hopelessness, difficulty bonding with the baby, and severe anxiety make this disorder extremely difficult to deal with while caring for a newborn.
Although Anxiety and Depression pertain to different disorders, there is general comorbidity between the two, meaning that both are likely to be present in one patient. Various research studies back up these claims, as professionals have found that 67% of individuals with Generalized Anxiety Disorder also reported Major Depressive Disorder in their lifetime, and 20% of individuals with Major Depressive Disorder also reported Generalized Anxiety Disorder in their lifetime.
Why do these disorders coexist at such a high rate? It’s a combination of many variables. There is a high overlap between the diagnostic criteria of anxiety disorders and depressive disorders. For example, symptoms in the diagnostic criteria of anxiety and depressive disorders include restlessness, insomnia or hypersomnia, fatigue, indecisiveness, and trouble concentrating. Additionally, both conditions fall under the same “common component” category of “general distress,” contributing to their overlap.
Several risk factors also influence how often anxiety and depressive disorders coexist. Researchers have found a strong correlation between the development of anxiety and depression and one’s genes. This correlation between genetics and the disorders remains despite differences in environment. The trait of neuroticism, classified by a disposition to experience negative emotions, is known to be a precursor for anxiety and depression. Studies have shown that genetic risk factors link neuroticism and these disorders, creating one big pool of possibilities for the development of anxiety and depression.
There are multiple types of medications available that help balance out the levels of neurotransmitters responsible for hormones that affect the mood, such as serotonin and dopamine. Finding a healthy balance may be the most significant factor in your journey to managing and diminishing the effects of anxiety and depression. Although no “best” anxiety and depression medication exists, some will work better for you than others, including factors like side effects, reliability, and effectiveness at controlling triggers or the severity of symptoms. It is essential to regularly consult with your doctor, both for help identifying proper medication to try, as well as assistance in evaluating long-term effectiveness.. Below are the most common medications that help with anxiety and depression, along with necessary information regarding their side effects and withdrawal symptoms.
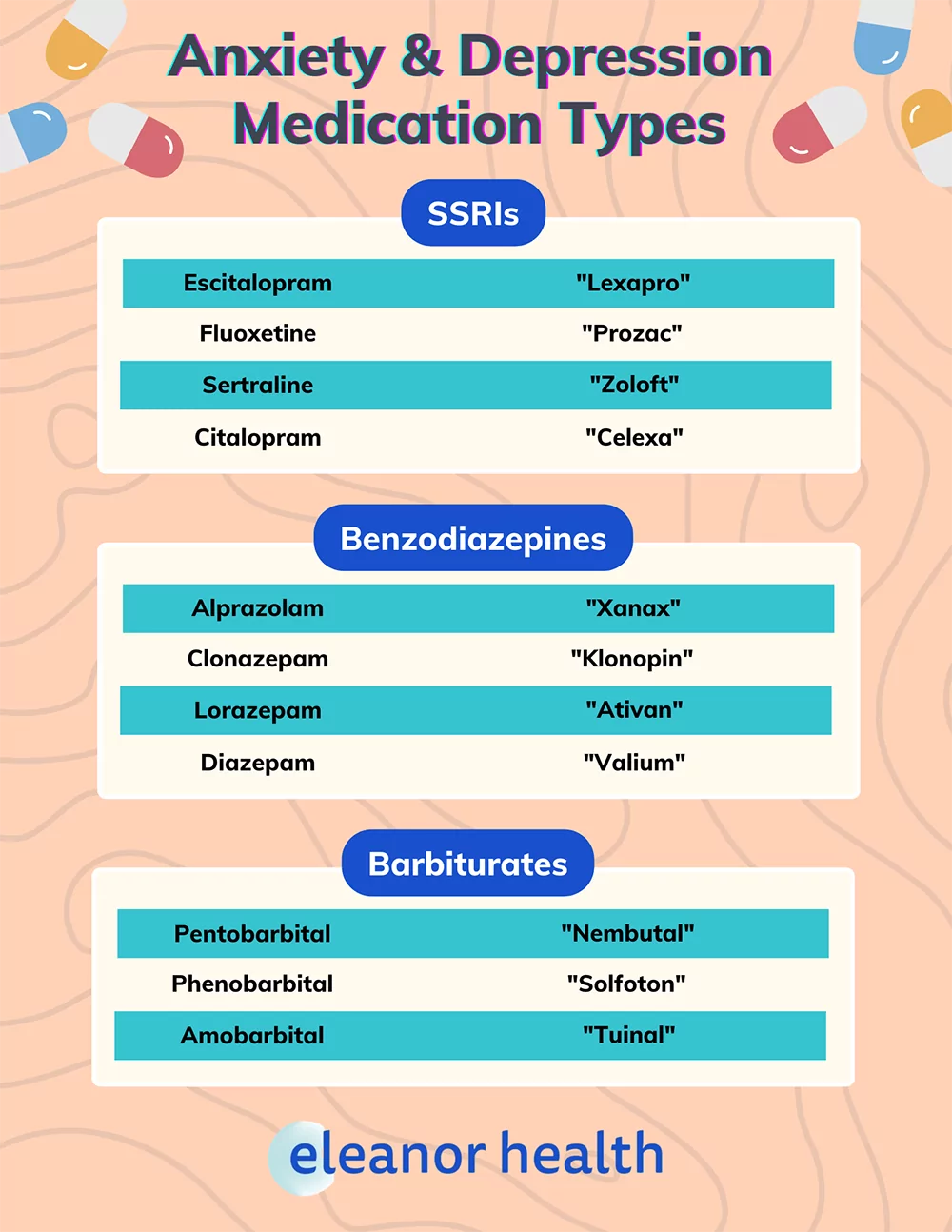
SSRIs are antidepressant medications popular for treating depression and anxiety disorders. They are often prescribed by doctors at low doses and gradually increase with time if needed. Serotonin is a neurotransmitter or chemical in the brain that regulates moods, cognition, memory, and other brain functions. Depression and anxiety are correlated with decreased levels of serotonin in the brain. As the name suggests, SSRIs increase serotonin levels in the brain, helping boost positive moods.
Common Brands: Lexapro (Escitalopram), Prozac (Fluoxetine), Zoloft (Sertraline), Celexa (Citalopram), and Paxil (Paroxetine).
Although SSRIs are generally safe and low in side effects, they can cause dangerous side effects in some instances. Fortunately, most people who take SSRIs only experience mild side effects (if any), which tend to subside the longer they are on the medication [1]. For example, people who are new to SSRIs may encounter mild side effects, like nausea, during the first few weeks of starting the medication, which subsides after more time passes.
Common/Mild Side Effects:
*may persist longer than the first few weeks of starting SSRI
It is necessary to continue taking the prescribed SSRI regularly, even if mild side effects persist. This is because SSRI medications take several weeks for you to benefit from their impact and see a difference in your levels of anxiety and depression [2]. By that time, the benefits of the medication and the improvement of feelings of anxiety and depression should outweigh the negatives of mild side effect(s).
Uncommon/Serious Side Effects:
*associated with “Serotonin Syndrome.”
If you experience serious side effects, contact your doctor immediately. They are uncommon but can be a sign of Serotonin Syndrome, which occurs when the level of serotonin in your brain becomes dangerously high. If you experience symptoms associated with Serotonin Syndrome, stop taking the medication and contact your doctor or emergency help immediately.
Cautions and Interactions: SSRIs can work wonders for some but can be wholly unsuitable and even dangerous for others. Your risk of potential issues depends on specific pre-existing conditions and interactions with other medications or substances [3].
If you have the following conditions and/or fall into the following categories, notify your doctor before starting SSRIs.
If you start an SSRI while taking the following medications or substances, your risk of interaction-caused side effects and Serotonin Syndrome increases.
While SSRIs aren’t known to be highly addictive, stopping your treatment abruptly or missing a few doses in a row can create withdrawal-like symptoms. These withdrawal symptoms are better known as “Antidepressant Discontinuation Syndrome.” They are relatively common, occurring in 20% of patients who quit their SSRIs all at once after at least six weeks of continued usage. This is because most SSRIs (excluding Prozac) have a short half-life, meaning that missing just a dose or two will likely abruptly diminish the SSRI concentration in the bloodstream. This, in turn, makes it more likely for the individual to experience distressing side effects comparable to withdrawal symptoms.
SSRIs can cause changes in the brain that affect serotonin receptors, creating a period of adjustment and withdrawal when medication is stopped abruptly. The brain will “down-regulate” the receptors, so there is a balance between serotonin and receptors, leaving a sudden decrease in serotonin and down-regulated receptors when treatment is stopped. You are likely to experience unpleasant side effects after this.
Common SSRI withdrawal symptoms are often described as “flu-like” symptoms or feeling the sudden re-emergence of anxiety and depression. Although these symptoms may be distressing, they are typically not severe. Common symptoms include:
*more rare/concerning symptoms. If you experience these, contact a doctor or professional immediately.

Anxiolytics are a type of medication typically used to treat anxiety but have also been researched to affect depressive symptoms positively. Because over 50% of people suffering from depression also suffer from anxiety, and vice versa, anxiolytics are often used to treat “anxious depression.” Additionally, researchers have found that anxiolytics frequently help with insomnia, a common symptom of depression. The three categories of Anxiolytics are:
“Benzos” are a type of medication that help calm your mind and relax your muscles during high anxiety. They can do this because the medication works by slowing down the brain and the rest of the central nervous system, which regulates how much sensory information the body takes in. By taking information in slower, the stress and overwhelm your body may feel will also subside. Benzos are usually not recommended to be used long-term because of their addictive nature and the increased risk of side effects.
Common Brands of Benzodiazepines: Xanax (Alprazolam), Klonopin (Clonazepam), Ativan (Lorazepam), Valium (Diazepam), and Chlordiazepoxide (Librium).
A sub-category of Benzos is Non-Benzodiazepines, which target the same symptoms and have the same side effects as benzodiazepines, except they have a different molecular makeup and therefore cannot be called the same title. They are commonly referred to as “Z-drugs” because the names of the most popular non-benzodiazepines all start with the letter “Z.”
Common Brands of Non-Benzodiazepines: Zolpidem (Ambien), Zaleplon (Sonata), and Zopiclone (Imovane).
Taking Benzodiazepine medication correctly and as regulated by your doctor is overall safe for short periods. However, they should not be taken long-term, even if you stick to the same prescription your doctor initially recommended. This is because they are designed for “short term relief” only, and taking them long-term could cause more severe side effects and risk of addiction.
Common/Mild Side Effects:
Uncommon/Serious Side Effects:
*Rarest side effects, speak to your doctor immediately.
**Common primarily in children and the elderly. Contact your doctor if side effects persist.
Cautions/Interactions:
Because Benzodiazepines cause sedation already, they can cause an increased and potentially dangerous amount of excessive sedation when used with other depressant substances, like alcohol, narcotics, and tranquilizers. For this reason, one should avoid depressant substances when taking Benzos, unless prescribed and carefully regulated. Other interactions include:
Taking Benzodiazepines at a high dosage and/or for an extended period is not recommended because of their addictive nature and intense withdrawal symptoms. It is easy to become tolerant to Benzos after taking them for a significant amount of time, meaning that the person becomes so used to the dosage they have been taking that they require a higher dosage to feel the same effects [7]. The higher the dosage and the longer the individual takes the medication, the stronger the withdrawal symptoms will be if they immediately stop or even wean off the medication.
There are two types of withdrawal associated with benzodiazepines. The first and more common of the two is often referred to as “rebound withdrawal”, and occurs 1-4 days after stopping taking the medication. Rebound withdrawal typically includes symptoms like solid bouts of anxiety and insomnia but doesn’t last long [8]. The second form of withdrawal may occur even after rebound withdrawal, which includes stronger withdrawal symptoms lasting about 10-14 days. These symptoms include “sleep disturbance, irritability, increased tension and anxiety, panic attacks, hand tremor, sweating, difficulty in concentration, dry retching and nausea, some weight loss, palpitations, headache, muscular pain and stiffness and a host of perceptual changes” [9].

This type of medication works similarly to benzodiazepines but is much stronger. They are known as “sedative-hypnotics” and are typically prescribed at very low doses because of their highly addictive nature. Higher dosages of particular Barbiturates are prescribed to decrease heart rate and blood pressure for those with heart health issues.
Common Brands of Barbiturates: Nembutal (Pentobarbital), Solfoton (Phenobarbital), and Tuinal (Amobarbital).
A subcategory of Barbiturates is Beta-blockers. Although this type of medication is typically prescribed for heart conditions, one type called Propranolol is commonly prescribed for intense anxiety symptom relief. Propranolol is used to treat co-occurring symptoms of depression and anxiety. However, it may also increase symptoms of depression like fatigue and lack of motivation because it slows down the heart rate. This is something to monitor and discuss with your doctor because the medication’s improvements to your depression should certainly outweigh the side effects.
Common Brands of Beta-blockers: Propranolol (Inderal) and Atenolol (Tenormin)
The side effects of Barbiturates have a wide range, depending on the prescribed dosage and longevity of usage.
Common/Mild Side Effects:
Uncommon/Serious Side Effects (signs of overdose):
Cautions/Interactions:
Like Benzodiazepines, one should not take Barbiturates along with other sedative substances. For Barbiturates to have their intended effect, and to avoid dangerous side effects, avoid these while taking prescribed Barbiturates:
Barbiturates are habit-forming and likely to create dependency, especially with higher dosages and longer usage periods. “Barbiturate Withdrawal Syndrome,” as many medical professionals call it, typically occurs 2-4 days after the drug is suspended. Symptoms can range from mildly concerning to fatal [10]. Therefore, a medical professional should always monitor withdrawal symptoms, and Barbiturates should be slowly weaned off instead of stopping all at once.
Withdrawal Symptoms:
*Serious withdrawal symptoms usually occur when initial withdrawal symptoms go untreated. Contact a medical professional immediately if you experience these.

People with anxiety and depression sometimes have co-occurring substance use disorders (SUDs). Prescription medications are a big component of SUD treatment, as they help stabilize patients who are having a hard time managing symptoms. However, some of these medications for SUDs can interact in negative ways with benzodiazepines and other medications that depress the central nervous system (CNS), like barbiturates.
People on medication-assisted treatment (MAT) for opioid use disorder (OUD) should be careful to avoid benzodiazepines and CNS depressants if they are also taking buprenorphine (or buprenorphine/naloxone).
The interaction between benzodiazepines and buprenorphine can cause respiratory depression and low blood pressure. It also raises the risk of overdose and increased sedation with cognitive impairment. The interaction between buprenorphine and CNS depressants poses the same risks.
Buprenorphine can be prescribed generically or under the brand name Suboxone, or Zubsolv and Sublocade (which also contain naloxone).
Benzodiazepines and CNS depressants are also known to interact poorly with methadone, another drug used to treat opioid use disorder. Taking either benzos or CNS depressants together with methadone can also cause respiratory depression, increased overdose risk and heightened sedation with impaired cognitive function.
Benzodiazepine and CNS depressant prescriptions can be really helpful for your mental health. But their interaction with the main medications used to treat opioid addiction can be very dangerous and potentially lethal. If you are considering MAT treatment for opioid addiction, your provider will discuss other medication options to address your anxiety or depression.
At Eleanor Health, we do not prescribe long-term benzos or CNS depressants to patients who are also in treatment for opioid use disorder. We work with patients to taper off benzos or CNS depressants, and introduce other safe medications to manage their mental health.
We monitor progress during this transition, supporting patients with therapy, peer support and empathic care. We know that changing medications can be scary, especially if you are doing well on the med that’s being tapered off. But we are here to help you find a way forward.
When considering the usage of prescribed medications to combat your anxiety and depression, you must communicate openly with your primary care physician regarding your options. Your health background has a great deal to do with the medication that will work best for you, so transparency with professionals is key to finding the most effective medication. Additionally, stay vigilant in keeping track of taking your medications and possible side effects. Contact your doctor immediately if you have any medication concerns. Remember, the pros should always outweigh the cons!
Eleanor Health is here to help you build your confidence and momentum towards the future you want. We provide treatment services for adults with alcohol, opioid, and other substance use disorders. We are currently located in Louisiana, Massachusetts, North Carolina, New Jersey, Ohio, Texas, and Washington.
 Natural Treatments for Depression: Can They Help?
Natural Treatments for Depression: Can They Help?
 What are SSRIs?
What are SSRIs?
 The Connection Between Depression and Sleep
The Connection Between Depression and Sleep