Note: Here at Eleanor Health, we believe that language surrounding addiction care should be positive, inclusive, and inoffensive to all affected. While this piece may use terms like “alcoholism” and “addiction” to connect the content with those who need it, we encourage the use of “alcohol use disorder” instead, which is a less stigmatized term. Learn more about how words matter in recovery by checking out our full-length post here.
Post Traumatic Stress Disorder (PTSD) and alcohol use disorder (AUD) are highly correlated. This means that people with PTSD are significantly more likely to develop a dependency on alcohol, and people with alcohol use disorder are more likely to be at risk of experiencing a traumatic event that leads to PTSD. Research has attested to this, as studies have shown that 1 out of every 10 Vietnam veterans with PTSD also had issues with alcohol, like binge drinking, that they had developed in response to trauma. This statistic is higher than the average individual who doesn’t experience PTSD. To get proper treatment for alcohol use disorder and PTSD, we must first learn more about their relationship. Keep reading to discover why comorbidity between these disorders occurs and the effective treatment options to help.
Post Traumatic Stress Disorder, or PTSD, is a mental health disorder that results from a majorly impactful, negative event. It is important to note that everyone has a different reaction to different experiences, so trauma won’t be developed in the same way for everyone. For example, someone may get into a car accident and develop PTSD, never being able to drive again. In contrast, another individual may not develop trauma and be able to drive the very next day. It all depends on the individual’s vulnerability, resilience, and pre-existing mental health conditions that can cause susceptibility to the development of PTSD. However, PTSD is relatively common, with about 8 million people experiencing the disorder in a given year [1].
The most common symptoms of PTSD are:
Although many individuals experience one or more of these symptoms after a distressing and traumatizing event, they typically subside after about a month. The continuation or worsening of symptoms after a month can be a clear sign of PTSD. If you are experiencing any of these symptoms more than a month after the event and/or are having thoughts about self-harm, contact your doctor immediately.
The symptoms of PTSD can be extremely distressing, often causing feelings of heightened anxiety and even hypervigilance (an elevated state of arousal in which one constantly assesses potential threats around them). People who suffer from these distressing symptoms may turn to alcohol to “numb the pain” their PTSD is causing.
People with PTSD may also turn to alcohol as a way to deal with physical symptoms. For example, a common symptom of PTSD and being traumatized in general, is having trouble falling asleep and staying asleep. Many individuals start using alcohol to help them “mellow out” and get into a more relaxed state to get a good night’s sleep. However, this often creates a dependency on alcohol. Additionally, over 65% of veterans experience chronic pain from their time in the war [2]. Because of this, it is also fairly common for veterans with PTSD to ease their chronic pain by self-medicating with alcohol.
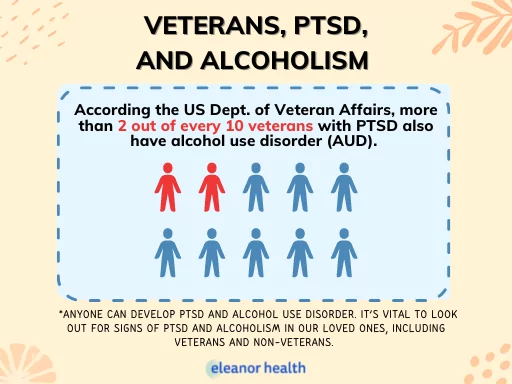
It is important to note that veterans are a particular community at higher risk for developing both PTSD and alcoholism. More than two out of every ten veterans with PTSD also have alcohol use disorder, and about 30% of veterans seeking treatment for alcoholism also have PTSD [3]. These statistics are higher than those of non-veterans.
However, as mentioned previously, anyone can develop PTSD and alcohol use disorder. This is why it’s vital to look out for signs of PTSD and alcoholism in our loved ones, including veterans and non-veterans.
Using alcohol as a coping mechanism can quickly become a disorder of its own. If one falls into an alcohol dependency, they will soon have to deal with the consequences of this disorder and their existing PTSD.
Using alcohol too frequently makes it harder to cope with PTSD symptoms and stress in general. In fact, many resources show that using alcohol can make anxiety and depression worse long term. Additionally, resources indicate that the use of alcohol typically makes PTSD treatment less effective [4].
In terms of PTSD, binge drinking can increase symptoms like feeling emotionally numb and disconnected from others, becoming irritable and reactive, and experiencing “jitters” and feelings of being “on guard” at all times. Not to mention, once someone creates a dependency on alcohol, it’s harder to stop without experiencing withdrawal symptoms. These withdrawal symptoms may be tough to deal with on top of existing PTSD symptoms.
If you think you may be experiencing PTSD and/or an alcohol use problem, it is always a wise decision to reach out to your doctor so you can talk about possible treatment plans.
A few examples of effective treatment options for those with PTSD and AUD are:
Trauma-Focused Cognitive Behavioral Therapy: TF-CBT helps people suffering from PTSD and addiction rewire negative thought patterns that may contribute to their disorders, focusing on the impact of trauma in their life. Here, they will learn healthier coping mechanisms for dealing with these disorders.
Support Groups for Trauma and Alcoholism: PTSD and alcoholism can influence an individual to isolate themselves, adversely causing feelings of depression. Support groups can help them feel understood and give them a way to recover alongside individuals in similar situations as them.
Medication: There are many different medications out there that help treat alcohol use disorder and PTSD. Speak to your doctor if you feel medication may be a promising treatment route.
If you are experiencing AUD and PTSD, we are here to help. Call us at 781-487-1070 or fill out this form to learn more.
You may be reluctant to reach out to a loved one to try to help with trauma and alcoholism for fear that you are overstepping a boundary. As long as you come from a non-judgmental, caring, and respectful place, reaching out to help a loved one will always do more good than harm. Your support may be just the thing they need to get professional help and start their recovery journey.
Here are a few tips and things to be mindful of when helping someone with PTSD and alcoholism:
When speaking to someone who has been traumatized, it is necessary to be cognizant of their trauma triggers. For example, if a previous romantic partner harassed your loved one, it is best not to bring up their dating life in conversation, as this will likely cause them to think about the traumatizing experience. Likewise, for someone in alcohol recovery, being around alcohol can be triggering. Be mindful of triggers and try your best to avoid them. Additionally, a negative stigma is attached to alcoholism and trauma, so be sure you speak to loved ones in a way that never involves victim blaming, judging, or assumptions.
Remember that your loved one may already know what they need to feel better. This may be to help them find treatment or someone to listen to them talk about their experience. Whatever support they need, express that you are always there for them and will help them.
Especially when dealing with someone’s trauma, it is essential to check in with our mental health and make sure that helping a loved one isn’t causing anxiety of our own. If you feel you are becoming triggered by your own trauma, or are too overwhelmed to be the main supporter of your loved one’s journey, take a step back. Referring your friend to a professional or another loved one that can be of better help to them is nothing to be ashamed of.
If you are seeking help with your loved one’s addiction, contact us today or complete our quick contact form below, to speak with an addiction treatment specialist.
If you need help with your substance use disorder, we are here to help you build your confidence and momentum towards the future you want. We are currently located in Louisiana, Massachusetts, North Carolina, New Jersey, Ohio, Texas, and Washington.
 How to Help a Loved One with Trauma
How to Help a Loved One with Trauma
 Therapy for Anxiety, Depression, Trauma: 3 Common Types
Therapy for Anxiety, Depression, Trauma: 3 Common Types
 5 Ways To Deal With Trauma
5 Ways To Deal With Trauma