Adult Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder affecting children and adults. It is characterized by difficulty staying focused or paying attention, impulsivity, and hyperactivity. According to the American Psychiatric Association, an estimated 2.5% of US adults have been diagnosed with ADHD.
While the symptoms of ADHD may be mild to moderate for some adults, others can experience significant impairment in functioning. A further complication arises when other comorbid (co-occurring) psychiatric conditions are present. This is often the case in adults with ADHD, as National Center for Biotechnology Information (NCBI) research indicates that 80% have at least one other psychiatric disorder.
Understanding the connection between ADHD and other disorders is critical for effective treatment. This article will explore common conditions that often present with ADHD, including anxiety disorders, mood disorders, autism spectrum disorder, learning disorders, and substance use disorders. We will also discuss treatment for co-occurring conditions to achieve the best possible outcomes.
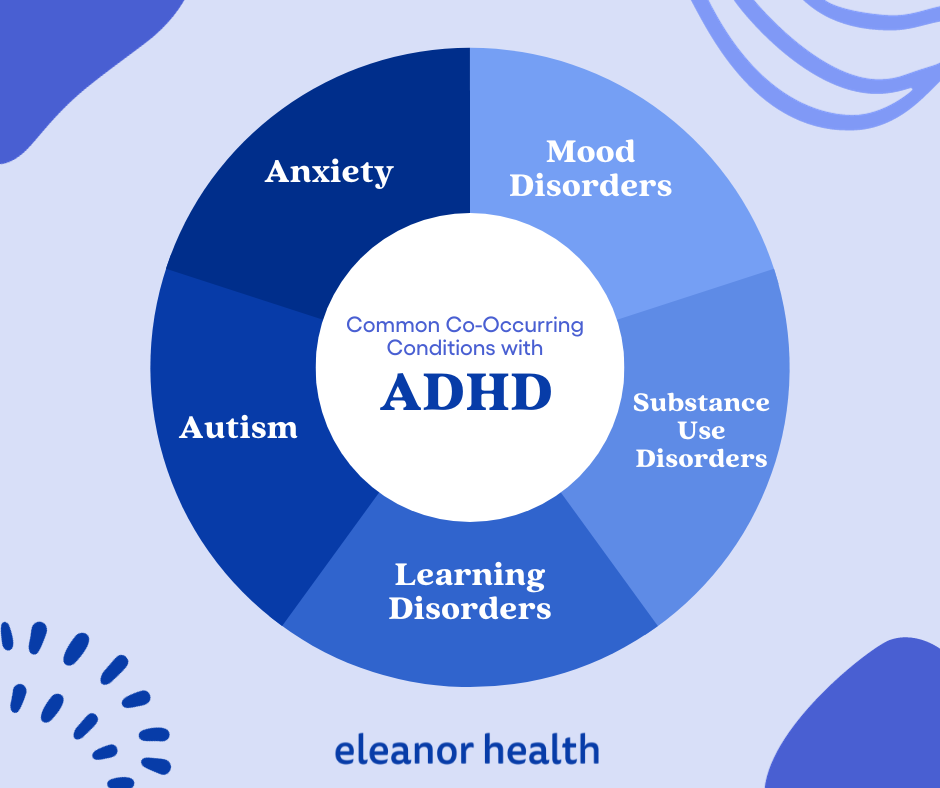
As stated earlier, many adults with ADHD have at least one or two additional psychiatric conditions. This is known as comorbidity, and it can amplify the symptoms of ADHD or mask them. For optimal symptom management, a thorough assessment is required. Recognizing the connection between ADHD and other mental health conditions is essential for receiving appropriate treatment.
Anxiety disorders are a group of mental health conditions that includes generalized anxiety disorder, social anxiety disorder, and panic disorder. According to the Centers for Disease Control and Prevention (CDC), 27.3% of Americans aged 18 and over have anxiety disorder symptoms in 2022. While anxiety can occur independently, it commonly presents with ADHD.
It is important to note that inability to focus and restlessness are symptoms that can occur in both ADHD and anxiety disorders and assessment by a mental health professional is required to determine if anxiety and/or ADHD are the correct diagnoses.
Adults with both anxiety disorders and ADHD tend to have more severe anxiety symptoms, earlier onset of anxiety, and more frequent additional comorbid psychiatric diagnoses than those who do not have ADHD. The presence of both ADHD and anxiety disorders can have a significant impact on an individual’s life, such as interfering with relationships, work performance, and/or academic achievement. Additionally, challenges posed by symptoms of ADHD can lead to the development of anxiety symptoms and anxiety can exacerbate symptoms of ADHD.
The first step in managing ADHD and co-occurring anxiety is to get a comprehensive assessment and diagnosis from a qualified mental health professional. Treatment may involve medication, psychotherapy and/or lifestyle changes.
Psychotherapy can help individuals learn skills to improve their ability to problem solve, organize, and regulate their anxiety. Medication can help individuals pay attention for longer, reduce impulsivity, lessen hyperactivity and manage anxiety. To note, many medications that improve focus can also exacerbate anxiety so it is important to work closely with a provider to best manage both ADHD and anxiety symptoms. Additionally, lifestyle modifications such as regular exercise, yoga and meditation can reduce stress, lessen worry and stabilize focus.
Mood Disorders are a group of mental health conditions that affect a person’s emotional state. These conditions include depression, bipolar disorder, and dysthymia. The National Institute of Mental Health (NIMH) estimated that 8.4% of U.S. adults aged 18 or older had at least one major depressive episode in 2020. That’s about 21.0 million adults with depression in the United States alone.
The co-occurrence of ADHD and mood disorders is well established; studies show that up to 40% of individuals with ADHD also have a mood disorder. Managing ADHD without appropriately stabilizing mood can lead to worse outcomes. Additionally, symptoms of depression such as hopelessness can develop when symptoms of ADHD are not controlled. Most importantly, symptoms of depression and bipolar disorder such as inability to concentrate, distractibility, talkativeness, impulsivity and restlessness are also common symptoms of ADHD, which can make diagnosis and treatment tricky.
Given the overlapping symptoms of ADHD and mood disorders, getting an accurate diagnosis from a qualified mental health professional is essential. This will ensure that the individual receives the most effective treatment plan tailored to their needs.
The main treatments for mood disorders and ADHD include medications and psychotherapy. Certain antidepressant and mood stabilizing medications can be beneficial for treating both ADHD and depression or bipolar disorder. It can also be beneficial to treat ADHD and mood disorders with multiple medications, when appropriate. Certain forms of psychotherapy, like cognitive behavioral therapy, can improve mood symptoms and cognitive functioning while also teaching skills for long term symptom management.
Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder characterized by difficulty with social interaction, communication, and repetitive behaviors. While 5.6 million children under 18 years have been diagnosed with ASD in the United States, 10.5 million adults are estimated to have the disorder, according to CFAH 2023 ADHD statistics & facts.
Both ADHD and ASD are considered neurodevelopmental disorders, meaning they are disorders that can arise during the development of the brain. Within this category there can be an overlap in symptoms and/or in presentation. Individuals with ASD struggle with social interaction, increased sensitivity to their environment, and inflexibility with changes and interests. Due to these symptoms, many individuals with ASD can appear to have ADHD or concurrently struggle with ADHD symptoms.
When symptoms of both autism and ADHD are present, developing a comprehensive treatment plan that addresses the individual’s unique needs is essential. Treatments may include medications, psychotherapy, lifestyle modifications, and/or other alternative therapies. In addition, support services can help individuals struggling with ASD and ADHD better manage their condition in a world designed for neurotypical brains.
While ADHD is not classified as a learning disorder, they often present concurrently. Learning disorders are defined as neurodevelopmental conditions that cause difficulty in processing information and using it to carry out tasks effectively. They include difficulties with reading, writing, math, and speech or language.
Learning disabilities and ADHD both fall in the neurodevelopmental category, with symptoms that can develop and present together. Learning disorders can affect an individual’s ability to prosper in our current society. This is especially true when the learning disorder co-occurs with ADHD, as both conditions can make it difficult to achieve success in typical school and work settings.
Common learning disorders associated with ADHD include dyslexia, dyscalculia, and dysgraphia. Dyslexia is a reading disorder that affects the ability to read and comprehend written words accurately. Dyscalculia is a math disorder that makes it challenging to work with numbers. Finally, dysgraphia is a writing disorder characterized by difficulty forming letters, using proper spacing between words, or organizing thoughts in written form.
Treatment options for individuals with learning disorders and ADHD often include psychotherapy, lifestyle modifications and accommodations. Psychotherapy and lifestyle modifications such as learning skills to improve focus, taking breaks to reduce stress and maximize productivity, and practicing mindfulness can make it easier to cope with symptoms. Additionally, accommodations can make a big difference in making tasks more manageable for individuals with ADHD and learning disabilities. These include extended time for tests, a quiet place to work, or using assistive technology.
An addiction or substance use disorder (SUD) is a chronic condition that is characterized by compulsive drug or alcohol use despite negative consequences. Individuals with an SUD are more likely to have a comorbid mental health condition including depression, anxiety, and ADHD. Studies have found that 23% of people seeking treatment for an addiction were also diagnosed with ADHD.
Individuals with ADHD struggle often with impulsivity which can lead to increased risk for using drugs or alcohol. Additionally, some substances can help those with ADHD improve focus but have abuse potential, which can lead people to self-medicate with drugs and possibly become addicted to them.
Treatment for individuals with ADHD and an SUD should focus on managing both conditions simultaneously. This could include a combination of medications, psychotherapy, lifestyle modifications, and self-care practices. To note, some medications to treat ADHD can have abuse potential and may need to be avoided for individuals struggling with addiction. In some cases, detox and residential rehab stays may be necessary to stabilize off a substance while working to manage symptoms of ADHD.
The most crucial step in managing ADHD and coexisting conditions is acknowledging the full impact these conditions can have on a person’s life. Taking stock of symptoms and how they are impairing daily or long term functioning and goals can help clarify what needs improvement. It is also essential to recognize any guilt or self-judgment associated with having both disorders so they can be dealt with head-on.
Today, more resources are available than ever to help individuals with ADHD and coexisting conditions deal with their symptoms. Individuals should reach out to a mental health provider to discuss their symptoms and receive a full assessment.
In addition, support groups and online forums can help those who struggle with symptoms find additional resources and support.
Once diagnoses are made, it is important to work closely with a provider to develop a comprehensive treatment plan. Plans should be personalized and can include non-pharmacological and pharmacological approaches to improving symptoms. Treatment plans that are most successful address all comorbid conditions.
Stress can exacerbate symptoms of ADHD and coexisting conditions, so it is important to practice regular self-care. This could include improving sleep quality, eating a balanced diet, exercising regularly, and engaging in relaxation activities such as yoga or meditation. In addition, you should reduce your exposure to environmental toxins like secondhand smoke and unnecessary stressors like overworking. Finally, tools like mindfulness can improve overall well being in addition to improving symptoms of almost all mental health conditions.
ADHD and comorbid mental health conditions are often chronic and relapsing symptoms can arise. Continued check-ins with a mental health provider along with adherence to treatment plans can reduce the risk for breakthrough symptoms. Keeping track of symptoms and noticing patterns that exacerbate or improve them can also prevent them from occurring.
Living with ADHD and coexisting conditions can be challenging, but it is possible to manage them effectively. Taking note of daily struggles, reaching out to start treatment, developing a plan, making lifestyle adjustments and putting in the effort over time are the best ways to manage symptoms and achieve success.
At Eleanor Health, we specialize in treating adults with Attention-Deficit/Hyperactivity Disorder (ADHD) and comorbid psychiatric conditions, including substance use disorders. More so, we offer compassionate, evidence-based care and strive to improve the quality, delivery, and accessibility of treatment. Contact us today to get started.
 ADHD Symptoms and Treatment
ADHD Symptoms and Treatment
 Therapy for Anxiety, Depression, Trauma: 3 Common Types
Therapy for Anxiety, Depression, Trauma: 3 Common Types
 Natural Treatments for Depression: Can They Help?
Natural Treatments for Depression: Can They Help?